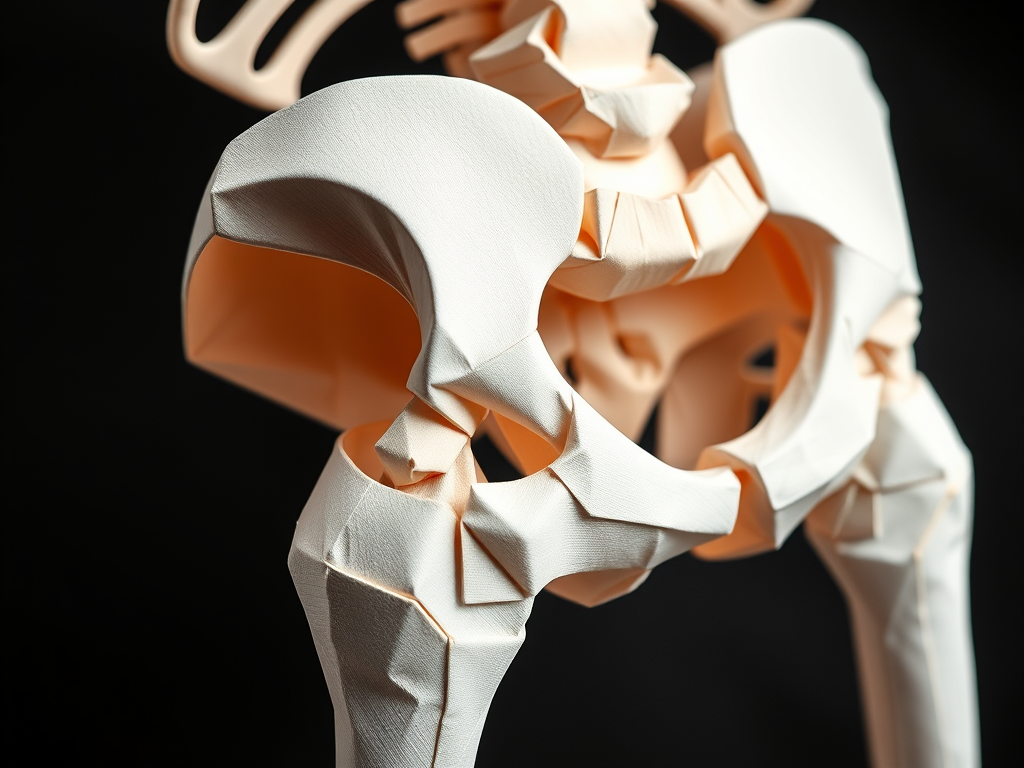
Understanding and Managing Adhesions After Hip Arthroscopy
Hip arthroscopy has become an essential procedure for addressing various hip pathologies, from labral tears to femoroacetabular impingement (FAI). However, with the growing number of these procedures comes an increase in patients requiring revisions due to complications like adhesion formation and loss of Range of Movement. Understanding the implications of adhesions and how to manage them effectively is vital for optimizing recovery.
What Are Adhesions?
Adhesions are bands of scar-like tissue that form during the healing process, often triggered by injury or surgical intervention or gross inflammation. While part of the body’s natural response to trauma, excessive adhesions can lead to:
- Pain and stiffness
- Mechanical symptoms such as clicking or catching or pinching pain
- Reduced range of motion (ROM)
- Microinstability, causing the hip joint to feel unstable when moving
These symptoms can significantly hinder post-surgical rehabilitation and compromise overall outcomes.
The Role of Physiotherapy in Preventing Adhesions
Physiotherapists play a crucial role in preventing adhesion formation by guiding patients through tailored rehabilitation programs. Key strategies include:
1. Early Mobilization to the right ROM and using just the right amount of movement
- Controlled, pain-free movements promote optimal tissue healing while preventing excessive scar tissue buildup, and stretching scarring in the right direction.
- Gentle ROM exercises should begin as early as the surgeon permits to maintain joint mobility, but need to be tailored to the patient and the surgical intervention they have had. Rotational and circumduction movements are the most useful.
2. Progressive Loading
- Gradual introduction of weight-bearing and strengthening exercises prevents stiffness while enhancing muscle support around the hip.
- Pay special attention to avoiding compensatory movements that could strain the healing tissues and cause load in the wrong tissues.
3. Manual Therapy Techniques
- Soft tissue mobilization to the capsule, joint mobilizations, and stretching can help reduce stiffness and improve circulation in the intraarticular areas as well as around the capsule and porthole area, but should be done in a controlled and prescriptive way.
4. Patient Education
- Teaching patients the importance of compliance with their rehab program is critical, and using strict timelines and understanding what movements that should be avoided especially, and how the healing timelines occur . Hyper extension control is vital in the 1st 16 weeks.
- Encourage them to report any signs of persistent pain, stiffness, or mechanical symptoms early.
- Bear in mind scarring and loss of ROM comes on as the healing progresses- so will not be in the 1st few weeks but can progress and worsen as they hit 4-6-8 weeks.
When Adhesions Form: Recognizing and Addressing the Issue
Despite preventative efforts, some patients may still develop adhesions. As physiotherapists, it’s essential to recognize the signs:
- Persistent stiffness beyond the expected timeline.
- Pain during certain movements or activities.
- Difficulty achieving full ROM despite adherence to therapy.
Rehabilitation After Surgical Lysis of Adhesions
Following a second surgery to address adhesions, the stakes are higher. The physiotherapy program must balance protecting the healing tissue with restoring function.
Key Focus Areas:
- Restore ROM: Initiate passive and active-assisted ROM exercises early to prevent new scar tissue from forming. Consider Continuous Passive Machine usage.
- Controlling excessive inflammation early on: consider using Game ready 3-4x a day.
- Strengthen Musculature: Gradual strengthening of the hip flexors, extensors, abductors, and core muscles improves joint stability.
- Functional Movements: Introduce exercises that mimic daily activities or sports-specific motions as the patient progresses.
- Continuous Monitoring: Watch for signs of recurrence, such as decreased ROM or pain flare-ups, and adjust therapy accordingly.
Current Trends and Research in Adhesion Prevention
Ongoing clinical trials are exploring innovative ways to reduce the risk of adhesion formation. Biologic agents, systemic medications, and advanced surgical techniques aim to mitigate the excessive healing response responsible for adhesions. Staying updated on these developments can help physiotherapists incorporate evidence-based strategies into their practice.
Takeaway for Physiotherapists
Adhesions after hip arthroscopy can be a challenging complication, but effective prevention and management can significantly enhance patient outcomes. Through early mobilization, progressive exercises, and consistent monitoring, physiotherapists can play a pivotal role in ensuring that patients regain pain-free mobility and function. By staying informed and adapting to advancements in care, you can help patients navigate their recovery journey with confidence and success.
NOTE: Collaboration with the surgical team and patient education are key components of effective post-arthroscopy rehabilitation. Together, we can help patients overcome the challenges of adhesion formation and achieve their rehabilitation goals.
Note: This blog is intended to provide practical insights for physiotherapists working with hip arthroscopy patients. Always tailor rehabilitation programs to individual patient needs and surgical guidelines.
Reference
Adhesions in the setting of Hip Arthroscopy
https://pubmed.ncbi.nlm.nih.gov/?term=Ruzbarsky+JJ&cauthor_id=37909708
Joseph J Ruzbarsky 1 2, Rui W Soares 3, Spencer M Comfort 1, Justin W Arner 4, Marc J Philippon 1 2
Intra-articular adhesions following hip arthroscopy:a risk factor analysis
